Don’t take tryptophan or 5-HTP until you’ve read this
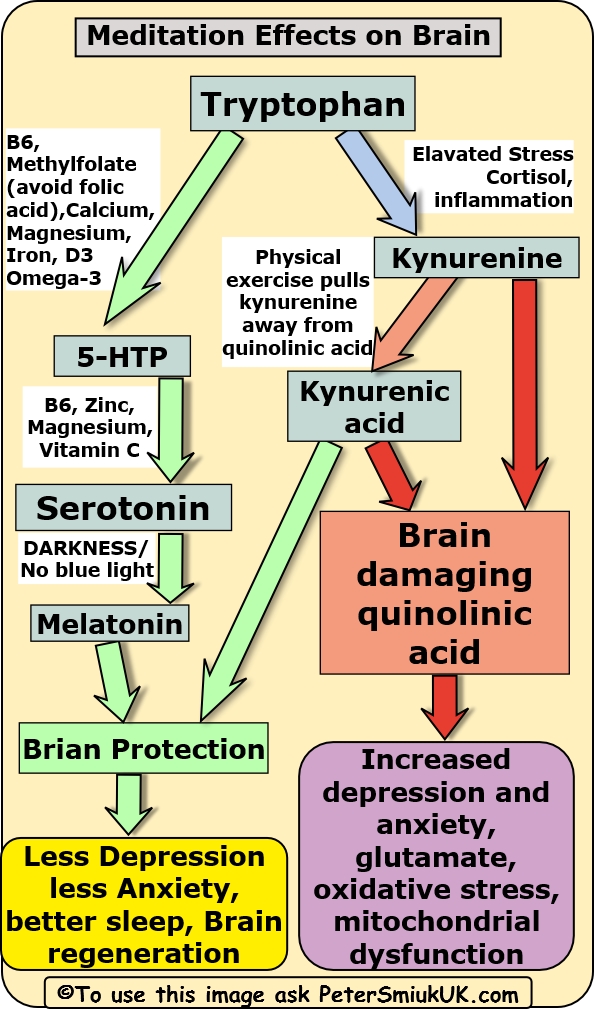
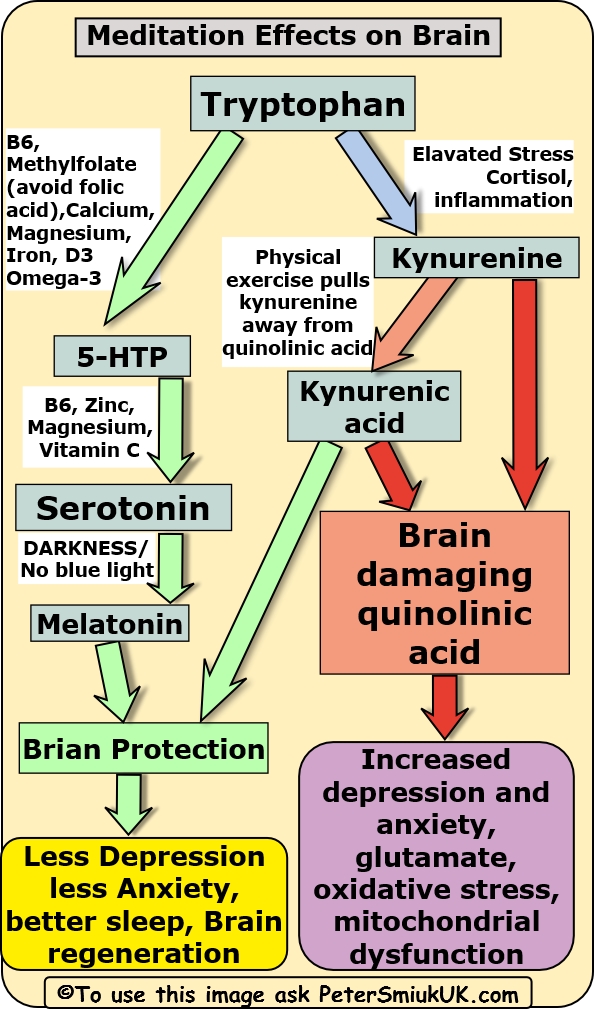
Tryptophan can be converted into antidepressant serotonin and brain protective melatonin, however it can go down another metabolic pathway forming first kynurenine which can be involved in activating immune cells and then the kynurenine can be converted into a highly neuro-toxic substance called quinolinic acid.
What determines whether tryptophan ends up making beneficial serotonin and melatonin or brain toxic quinolinic acid is determined by a number of factors including the presence of nutritional deficiencies, our levels of stress, inflammation and physical exercise.
Quinolinic acid promotes depression, anxiety bipolar mania and schizophrenia[i], it over stimulates the brain by inhibiting NMDA receptors[ii] producing excessive glutamate activity. Quinolinic acid also causes increased oxygen free radical damage and mitochondrial dysfunction.
How do we steer tryptophan towards the serotonin and melatonin that we want and away from toxic quinolinic acid
Whether tryptophan goes down the healthy pathway to make serotonin and melatonin or the unhealthy pathway to make quinolinic acid depends on 2 primary factors:-
- being deficient of essential nutrient cofactors needed to convert tryptophan into serotonin and melatonin
- increased levels of inflammation in the brain which can be caused by elevated stress and cortisol, hidden infections activating the immune system, a poor diet that promotes inflammation and more.
- When stress and inflammation steer tryptophan towards quinolinic acid tryptophan is first made into an intermediary substance called kynurenine and is one more thing we can do to prevent the tryptophan ending up being made into brain damaging quinolinic acid which is vigourous aerobic exercise. Vigourous exercise stimulates the muscles to convert kynurenine away from quinolinic acid and converted into a substance called kynurenic acid.
1. Nutrient Deficiencies
If you are deficient in vitamin and mineral cofactors needed to convert tryptophan into serotonin then this will steer tryptophan down the neurotoxic pathway to make quinolinic acid, and deficiencies in some of these nutrients such as vitamin D3 and magnesium are very commonplace, you could have the right now without even knowing it.
It’s simple to prevent the problem of deficient nutrient cofactors simply by a comprehensive multivitamin/multimineral containing B6, D3, zinc and methylfolate together with a separate additional magnesium supplement because a multiple mineral could never have enough magnesium in it without the tablet becoming too large. If you are severely deficient of D3 then you should probably spend a couple of weeks building up your D3 status prior supplementing tryptophan/5 HTP.
2. Inflammation in the Brain and Stress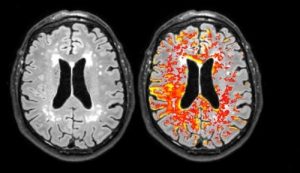
The other known factor that will steer tryptophan down the neurotoxic pathway is elevated levels of inflammation in the brain, in fact it is now known that inflammation in the brain is one of if not the primary driving force causing a variety of mental health problems from depression through OCD to bipolar and schizophrenia. Obviously these are different conditions involving different circuits and regions of the brain but inflammation is now known to be a common denominator in all of these conditions causing a breakdown in the key structures involved in each of these conditions; whether a person will develop one condition or another depends upon genetics, epigenetics and other factors.
Inflammation can come from a variety of courses from infections, injuries and again nutrient deficiencies and each of these has to be corrected and eliminated to get rid of the inflammation pushing tryptophan down the harmful quinolinic acid pathway. From the research it appears however that the most common cause of inflammation in the brain at least with regard to depression is prolonged elevations in stress levels.
3. Exercise and the kynurenine pathway
In my practice I’ve seen several patients suffering from severe depression that seemed to begin as soon as they stopped doing large amounts of vigourous aerobic exercise. They were all people with highly stressful jobs and lives and in my opinion inherently highly stressed nervous systems but they also did above average levels of vigourous aerobic exercise, such as running marathons et cetera. It appeared and I hypothesised that their brain could cope with the inflammatory effects of the high levels of stress as long as they maintained the exercise which was presumably steering kynurenine away from quinolinic acid. Unfortunately when they suffered a knee or some other injury that meant they had to stop exercising they suddenly developed severe clinical depression.
My treatment strategy was primarily to change the way their body managed stress physiology with brain training exercises and also combat inflammation with natural remedies and an anti-inflammation diet.
Hypothermia Antidepressant Treatment
a fascinating new avenue of research is that we can combat inflammation in the depressed brain by whole-body immersion in a high heat environment such as a sauna or hot bath. It seems the depressed brain is stuck in a semi feverish inflammatory condition and that by pushing the body temperature up into a high fever state (briefly and under safe controlled conditions I must add) then we can counteract this high temperature feverish state that causes damage to delicate brain structures. I discuss hypothermia antidepressant treatment elsewhere.
Stress blocks serotonin production and promotes neurotoxic quinolinic acid production
To be specific when I say stress levels I’m referring to the internal stress responses our body makes changes in our nervous system and hormonal system. I’m not referring to external stress levels in the outside world, because some people produce a very internal stress response even when there isn’t very much real stress in the outside world compared to other people that stay relatively calm and internally unstressed despite there being significant stress in danger in the outside world.
As far as producing inflammation in the brain the most significant internal stress response is the release of cortisol from the adrenal glands when the hypothalamus-pituitary-adrenal pathway (HPA axis) is over activated.
When increased threat levels are detected by the brain signals are sent to the hypothalamus which then sends a hormonal signal to the pituitary which send a hormonal signal to the adrenal glands to release the stress hormone cortisol. Cortisol easily crosses the blood-brain barrier and in the brain it increases production of cytokines which switch on the brains inflammatory immune response. If this only happened once in a while when it’s appropriate because we are in real danger that would be okay, but when we have chronic over activation of the HPA axis it causes persistent harmful levels of inflammation in the brain. Chronic over activation of the HPA axis may be a consequence of a history of trauma particularly in early life, some people are born with a highly strung and nervous system so to speak and of course a prolonged period of relentless increased life stress.
Interestingly the hypothalamus can’t tell the difference between real threat and danger or imagined threats and danger, as far as it is concerned it doesn’t matter whether the threat is real because we really are in currently in a real-world dangerous situation or whether the increased threat and stress levels are entirely created in the mind, the product of stressful psychology and remembering past traumas; if the hypothalamus the centre signal that we are under danger it activates the HPA axis.
The good news there are things that we can do to change the way our brain manages stress and stopped overactivity in the HPA axis causing the inflammation that both disrupts serotonin and other neurotransmitter production and also damages delicate structures in the brain that control mood. To learn about these techniques see: Overcoming Depression How to Stop Stress Causing Depression
REFERENCES
- Prog Neuropsychopharmacol Biol Psychiatry. 2011 Apr 29;35(3):702-21. doi: 10.1016/j.pnpbp.2010.12.017. Epub 2010 Dec 23. The new ‘5-HT’ hypothesis of depression: cell-mediated immune activation induces indoleamine 2,3-dioxygenase, which leads to lower plasma tryptophan and an increased synthesis of detrimental tryptophan catabolites (TRYCATs), both of which contribute to the onset of depression. Maes M et al PMID: 21185346 DOI: 10.1016/j.pnpbp.2010.12.017
- 2008 May;11(3):198-209. doi: 10.1080/10253890701754068. A link between stress and depression: shifts in the balance between the kynurenine and serotonin pathways of tryptophan metabolism and the etiology and pathophysiology of depression. Miura H, et al PMID: 18465467 DOI: 10.1080/10253890701754068.
- Mol Psychiatry. 2007 Nov;12(11):988-1000. Epub 2007 Apr 24. The immune-mediated alteration of serotonin and glutamate: towards an integrated view of depression. Müller N et al PMID: 17457312 DOI: 10.1038/sj.mp.4002006
[i] Journal of Affective Disorders 102 (2007) 65–72 Tryptophan breakdown pathway in bipolar mania. Aye Mu Myint et al. Available online 30 January 2007
[ii] FEBS J. 2012 Apr;279(8):1356-65. doi: 10.1111/j.1742-4658.2012.08485.x. Epub 2012 Mar 27. Quinolinic acid, the inescapable neurotoxin. Guillemin . PMID: 22248144 DOI: 10.1111/j.1742-4658.2012.08485.x